Crohn’s Disease Medicine Works to Treat EBA Patient, 36: Case Study

Omalizumab
A 36-year-old woman with epidermolysis bullosa acquisita or EBA — a non-genetic type of epidermolysis bullosa (EB) — was successfully treated with ustekinumab, an approved therapy for Crohn’s disease and other conditions, a case study reported.
Although the patient also had Crohn’s, an inflammatory condition of the digestive tract, her response to this medication did not correlate with the response to that disease, according to researchers.
The findings suggest that ustekinumab may be an effective treatment for EBA.
Epidermolysis bullosa acquisita “is notoriously resistant to treatment,” the team wrote. “Here, we present the first documented case of complete EBA control following topical corticosteroids/tacrolimus [medicated ointment] in combination with ustekinumab treatment for coexisting [Crohn’s disease].”
The case study, “Epidermolysis bullosa acquisita treated with ustekinumab: A case report,” was published in the journal SAGE Open Medical Case Reports.
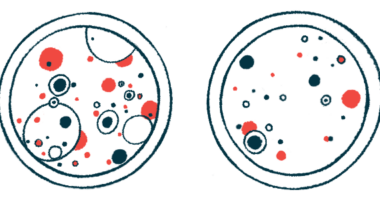
EBA is a non-inherited form of epidermolysis bullosa caused by a mistaken immune attack against type VII collagen, a protein that plays an essential role in attaching the top layer of the skin, or epidermis, to the dermal layer underneath.
The disease is characterized by blistering in layers of the skin in response to injury. It primarily affects the mucous membranes that line the mouth, nose, and eyes, but blisters also occur on the hands, elbows, feet, knees, and buttocks. The rare autoimmune disorder is mainly managed by preventing skin blisters, promoting healing, and the use of immunosuppressive and immunomodulatory agents.
EBA linked to Crohn’s disease
EBA has been associated with several inflammatory diseases, including Crohn’s disease (CD) — a type of inflammatory bowel disease (IBD) that causes chronic inflammation of the gastrointestinal tract.
In this report, researchers at McGill University, in Québec, Canada, describe the first documented case of EBA that was successfully treated with topical immunosuppressants combined with ustekinumab — an approved Crohn’s disease medication sold under the brand name Stelara. The patient had been diagnosed with both EBA and Crohn’s disease.
“To our knowledge, no studies exist reporting the effective treatment of EBA with ustekinumab, a humanized monoclonal antibody for the treatment of CD,” the team wrote.
The woman had a one-year history of Crohn’s disease, managed with daily doses of prednisone, an anti-inflammatory corticosteroid. She was treated at a dermatology clinic after a seven-year history of recurrent painful blisters, tiny bumps, and scarring on the back of her hands, feet, elbows, and knees.
Physical examination revealed non-inflammatory fluid-filled skin blisters, loss of the skin’s top layer, a lack of pigmentation, and scarring on injury-prone sites.
A biopsy of skin tissue in and around the damage showed subepidermal fluid-filled sacs and separation between the epidermis and dermal layers. Antibodies also were detected at the epidermis-dermis interface.
Blood tests revealed the presence of antibodies against type VII collagen. As a result, the woman was diagnosed with EBA and counseled on preventing skin injury. She also was prescribed the topical corticosteroid clobetasol propionate ointment alternating with tacrolimus ointment, which decreases the activity of the immune system.
One month later, she was started on intravenous (into-the-vein) ustekinumab by her gastroenterologist because her Crohn’s disease was not controlled by prednisone. She received an initial dose of ustekinumab followed by regular doses every eight weeks.
Assessment by the dermatologist two months after starting ustekinumab revealed marked improvement of her EBA, with few new lesions. Due to ongoing Crohn’s disease, the ustekinumab dose and frequency were increased.
At a reassessment eight months after starting ustekinumab, she reported complete control of EBA as evidenced by the absence of newly developing blisters and injury. She only had signs of her previous EBA skin damage.
Notably, her EBA response to ustekinumab did not correlate with the Crohn’s disease response.
“Further studies are necessary to clarify the common role of [type VII collagen] autoantibodies in CD and EBA, which may explain their common response to ustekinumab,” the researchers wrote. “Despite limitations imposed by the observational nature of this case report, ustekinumab may be an effective therapy for EBA.”
“Moreover, the successful treatment of the described patient’s EBA by ustekinumab further highlights the interplay between CD and EBA,” the researchers added.