Researchers Identify a Blood Biomarker for Epidermolysis Bullosa-associated Squamous Cell Carcinoma
Written by |
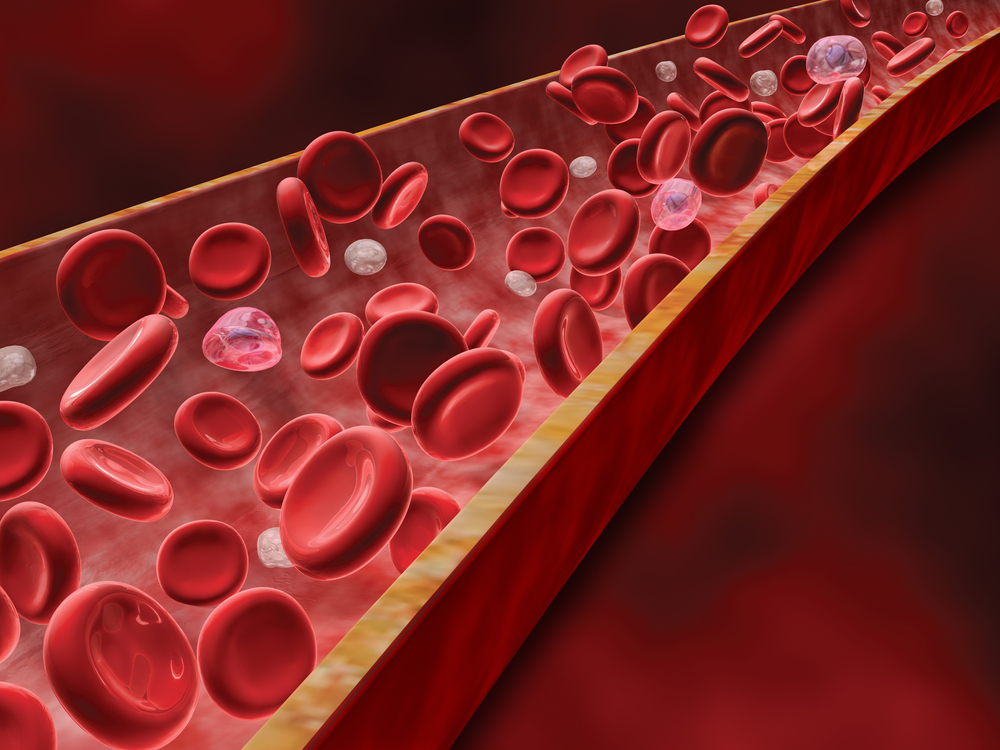
Using a simple blood sample may be sufficient to detect a biomarker for skin cancer in epidermolysis bullosa patients, a new study suggests. This is because the cancer-specific variant of the SLCO1B3 gene is found exclusively in extracellular vesicles detected in blood circulation.
The study reporting the findings is titled “Extracellular Vesicles as Biomarkers for the Detection of a Tumor Marker Gene in Epidermolysis Bullosa-Associated Squamous Cell Carcinoma.” It was published in the Journal of Investigative Dermatology.
Currently, diagnosing a tumor requires invasive biopsies in which clinicians use a needle to collect tissue for posterior analysis.
Extracellular vesicles are membrane spheres released by almost every cell type in the body. They are filled with proteins, lipids, DNA, and RNA. The content of vesicles reflects that of the cell of origin, so that tumor cells release vesicles carrying a tumor-specific signature.
This is the basis for using tumor-derived extracellular vesicles circulating in the blood as potential “specific biomarkers that can be utilized for cancer detection and diagnosis, as well as to gain insight into the biology of the tumor,” researchers wrote.
In the study, they explored the feasibility of using tumor-derived extracellular vesicles as a form of liquid biopsy to detect a recently described tumor biomarker gene, a cancer variant of the SLCO1B3 gene, for epidermolysis bullosa-associated squamous cell carcinoma.
They measured the expression of the cancer-specific variant of SLCO1B3 gene and found that it was only expressed in cell lines or tumor biopsies from squamous cell carcinoma patients.
“These data demonstrate that Ct [cancer-type]-SLCO1B3 is a tumor marker gene in RDEB-SCC [recessive dystrophic epidermolysis bullosa-squamous cell carcinoma],” researchers wrote.
The team then investigated if the cancer variant of SLCO1B3 was also found in extracellular vesicles. Results showed that the variant was found exclusively in tumor-derived extracellular vesicles, suggesting a potential use as a biomarker for squamous cell carcinoma screening in this patient population.
Researchers assessed its potential diagnostic value in an in vivo setting by injecting tumor cells into mice. After mice developed a sizable tumor, they were euthanized and blood samples were collected. Blood from mice that had not received tumor cells served as controls.
After extracting extracellular vesicles present in the blood from each group of animals, the researchers confirmed once again the presence of the cancer variant of SLCO1B3 only in vesicles from tumor-bearing mice.
Based on these results, the team concluded that “our data establish Ct-SLCO1B3 as a robust and reliable tumor marker in RDEB-SCC that could be exploited as a biomarker for this cancer.”
They also showed that the analysis of blood-circulating extracellular vesicles may be used as a minimally invasive strategy to detect cancer in these patients, “particularly once it has metastasized beyond the skin.”