Skin-derived stem cells promoted wound closure in RDEB: Study
Mesenchymal stromal cells are emerging as promising RDEB treatment strategy
Written by |
Skin-derived stem cells enhanced wound closure in people with recessive dystrophic epidermolysis bullosa (RDEB), according to clinical trial data.
The treatment reduced the occurrence of new wounds, extended the time that they recurred, and wounds that did not fully close got smaller. A larger clinical trial using a control group is needed to confirm these findings, the researchers recommended.
The clinical trial analysis was published in Cytotherapy, in the study, “ABCB5+ mesenchymal stromal cells facilitate complete and durable wound closure in recessive dystrophic epidermolysis bullosa.”
The COL7A1 gene encodes for a portion of the type VII collagen protein that helps provide structure and support to organs and tissues, including the skin. In RDEB, skin layers are weakly connected due to defects in that gene, leaving skin fragile and prone to blisters.
Mesenchymal stromal cells (MSCs), or mesenchymal stem cells, are a promising RDEB treatment strategy because they can travel to damaged tissues, boost tissue regeneration, and reduce scarring. MSCs can be isolated from the bone marrow or the umbilical cord.
MSCs from the skin, called dermal MSCs, carrying the protein marker ABCB5, have also been shown to have regenerative potential. In preclinical mouse studies, dermal MSCs outperformed bone marrow MSCs in migrating toward and integrating into wounds.
A recent open-label Phase 1/2a clinical trial (NCT03529877 and EudraCT 2018-001009-98), sponsored by Rheacell, showed dermal MSCs infused into the bloodstream significantly reduced disease activity, itch, and pain in 16 RDEB patients.
In this report, Rheacell scientists, collaborating with researchers in Germany, the U.S., the U.K., and Australia examined wound healing in patients who participated in the trial.
“We present a unique analysis in which we evaluated all wound types and followed up the durability of achieved wound closure up to more than 9 weeks,” the researchers wrote.
Times till wound closure
During the trial, participants received three infusions of dermal MSCs on days 0, 17, and 35. Affected body regions were photographed for documentary purposes at each visit, and 12 weeks later (three months). For this study, the photos were assessed by a wound care specialist alongside independent reviewers.
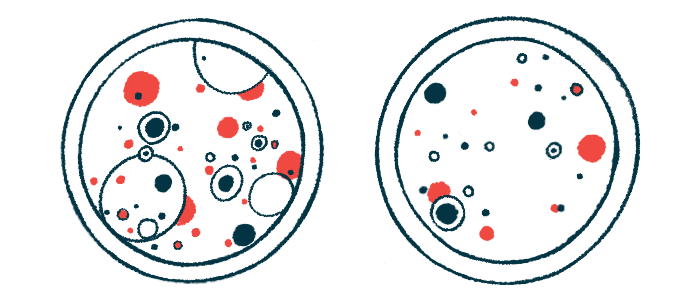
Overall, 168 wounds were included in the pre-treatment (baseline) analysis. During treatment, the average number of wounds decreased significantly by 28% on day 17, 51% on day 35, and 66% at 12 weeks.
The median time to the first wound closure was 35 days, which, according to researchers, was shorter than published control data, suggesting dermal MSCs infusions have “increased the velocity of wound healing.”
On day 17, 45 (26.8%) of the 168 wounds recorded at baseline had closed, and of them, 31 wounds were closed on subsequent visits, while the remaining had reopened. On day 35, 82 (48.8%) baseline wounds were closed, of which 69 (84.1%) were closed by week 12.
Lastly, 127 (75.6%) baseline wounds showed their first closure within 12 weeks. After 12 weeks, 109 (64.9%) baseline wounds had fully closed.
During treatment, “a greater proportion of wounds have healed as can naturally be expected within 12 weeks, suggesting that the treatment has stimulated chronic, otherwise nonhealing wounds to close,” the researchers wrote.
Regarding closure durability, of the 109 wounds closed after 12 weeks, 69 (63.3%) had already closed by day 17 and day 35. Conversely, 93 baseline wounds first showed closure up to day 35, and among these, 69 wounds (74.2%) were still closed by 12 weeks.
To measure wound size, the researchers applied a rating scale — from -3 to 3 — wherein a higher positive value indicated a smaller wound size and a negative number reflected enlarged wounds compared with baseline.
On day 17, the median change in wound size score was 1.4, 1.8 by day 35, and 1.9 at 12 weeks, all statistically significant improvements. Smaller but similar results were seen across wounds that had never closed by week 12.
Median new-wound development (wounds per day) dropped significantly by 79.3% between days 0 to 17 and days 35 to week 12. Likewise, new daily wounds fell by 76% between days 17 to 35 and days 35 to 12 weeks.
“In addition to previously reported effects on RDEB disease activity, itch and pain, systemic treatment with ABCB5 [positive] MSCs is capable of facilitating wound closure, prolongating wound recurrence, and decelerating the formation of new wounds,” the researchers said. “A larger trial with a randomized, placebo-controlled design, a longer efficacy period covering more MSC doses and refined pre-defined outcome parameters using standardized photography is needed to confirm these conclusions.”