Collagen Vesicles Released by Bone Marrow Stem Cells May Explain Their Therapeutic Potential, Study Shows
Written by |
Collagen type VII-filled vesicles released by bone marrow-derived mesenchymal stem cells may explain the therapeutic benefits of these cells in recessive dystrophic epidermolysis bullosa (RDEB), a study suggests.
The study, “Dual mechanism of type VII collagen transfer by bone marrow mesenchymal stem cell extracellular vesicles to recessive dystrophic epidermolysis bullosa fibroblasts,” was published in the journal Biochimie.
Recent clinical trials have shown that stem cells from the bone marrow, called bone marrow-derived mesenchymal stem cells (BM-MSCs), administered either intravenously or intradermally (within the skin layers), improved wound healing in patients with RDEB.
The mechanisms underlying this therapeutic effect are unknown.
Researchers hypothesized that BM-MSCs may secrete type VII collagen – whose levels are reduced or even absent in patients with RDEB – in spheres (vesicles) released to the cells’ environment.
To test their hypothesis, the team collected fibroblasts — cells that synthesize the extracellular matrix and collagen that support tissues — from patients diagnosed with RDEB.
As expected, the cells had lower levels of type VII collagen compared to normal human dermal fibroblasts.
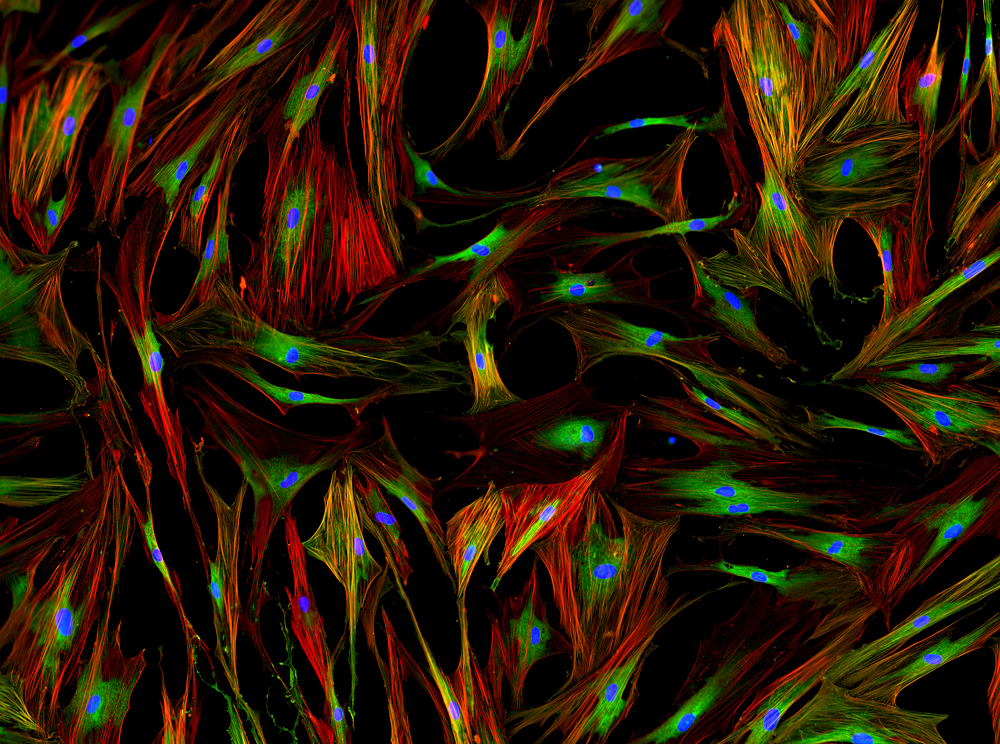
The team then cultured RDEB fibroblasts together with BM-MSCs in vitro and observed that BM-MSCs released extracellular vesicles that were transferred to RDEB fibroblasts. This transfer was detected within 24 hours of co-culture.
Researchers tracked the vesicles by staining BM-MSC cells with a fluorescent dye before co-culturing them with the RDEB fibroblasts. This means that the vesicles released from BM-MSCs had a specific color when analyzed under the microscope. The recipient, RDEB fibroblasts, were also stained with a different fluorescent marker.
Researchers then collected the extracellular vesicles released by BM-MSCs in vitro and found that they contained the RNA molecule needed to produce type VII collagen. This meant that the content of the vesicles, filled with genetic information to produce type VII collagen, once delivered to the RDEB recipient cells could lead to an increase of this missing protein.
Researchers found a significant increase in messenger RNA of type VII collagen after incubating RDEB fibroblasts with BM-MSC extracellular vesicles for 36 hours.
Using increasing amounts of BM-MSC extracellular vesicles they saw a corresponding increase in messenger RNA of type VII collagen in RDEB fibroblasts, confirming that the transfer of genetic information from the vesicles to the cells led to an increase in the protein levels of type VII collagen.
Overall, the team concluded that “our results support a model in which BM-MSC EVs [extracellular vesicles] help increase type VII collagen levels available to recipient cells by 1) donating BM-MSC type VII collagen protein and 2) inducing RDEB fibroblasts to make their own type VII collagen protein.”
“These findings allow us to hypothesize that the secretome [the molecules secreted by a cell] of BM-MSCs could have therapeutic value in the treatment of RDEB-related skin disorders,” the researchers stated.