The Difficult Decision in Favor of a Feeding Tube, Part 1
Written by |

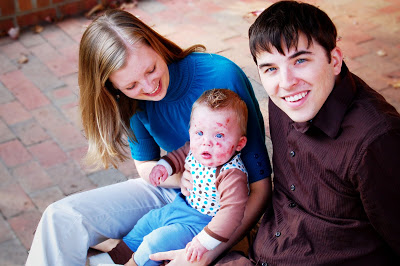
(Courtesy of Patrice Williams)
First in a two-part series.
Our son Jonah, who was born with junctional epidermolysis bullosa in 2009, struggled to eat from the beginning. It was one of the main reasons he had to remain in the NICU after he was born.
Jonah finally ate just enough to go home, but each day, it became more and more of a struggle. Some days, his lack of eating was due to being on pain medication. Some days, it was due to pain. Some days, it was blistering on his tongue. Some days, it was congestion. If there was a reason not to eat, he had it.
I recall one day in particular he woke up with a huge — think golf ball-sized — blister on the back of his tiny tongue. He definitely couldn’t latch or suck a bottle. Honestly, I’m not even sure how he could breathe.
I struggled and prayed and cried. What could I do? Did I try to hold this baby down and stick a needle halfway down his throat and attempt to drain it? If I did, would I cut him? Would he aspirate on the fluid? If I didn’t, would he choke in his sleep?
I put him down for a nap that day and packed a bag for the hospital while he slept. I prayed the whole time. When he woke up, the blister had drained and he was able to eat just enough. Another close call.
Even when he did eat, he had horrible acid reflux. This is common for people with epidermolysis bullosa. Even with medication and thickening his formula, eating was excruciating for him. He would cry and fight, and often it would take him more than 45 minutes to drink a bottle. If he did manage to get some formula down, most times he would throw it up.
I remember crying on my hands and knees on my kitchen floor trying to scoop up his vomit to measure how much it was, to see if he had kept anything down. It got so bad that he vomited at the sight or smell of food, and even if he just felt anxious. He threw up almost every time we laid him back in his infant car seat. Also, at his first Wake Forest basketball game, which you can read about here, as I don’t want to talk about it.
By the grace of God and a bunch of calorie-boosting additives, Jonah stayed on his growth curve. If I go back now and look at the binder where I tracked every ounce and calorie, I’ll almost have a PTSD response.
Between his pain and aversion to food, Jonah began only “dream feeding” when he was half asleep. It was the only time I could get him to take a bottle.
Worst came to worst as Jonah approached 1 year old. He was napping, and therefore feeding, less and less. Anytime he got the least bit congested, he’d stop eating altogether.
Several times he was at the point of dehydration, and we had our bags packed to head to the hospital. One time, we actually ended up in the emergency room, and while there, he finally decided to drink a small bottle of Pedialyte and a few ounces of a bottle. Never mind that I had tried that and all the things at home before giving up and taking him in. He thought he was hilarious.
We both had enough. He was still on his growth curve and miraculously gaining weight, but every day was a battle. I was literally force-feeding him. He hated it, and I was losing my mind. Both of us often were in tears. We knew this was a struggle for many EB kids, and we knew that for us, it was time for a gastrostomy feeding tube, or G-tube.
To this day, the decision to get a G-tube may be the scariest decision we have ever had to make for Jonah. We knew he needed it, but because he wasn’t “failure to thrive,” it was considered elective.
I was “electing” to have my EB child, whose trachea and esophagus would blister with the least friction, intubated. I was “electing” to have him taken into the operating room. I was “electing” to have doctors and nurses who knew very little about EB touch him. I was “electing” to put him in danger to keep him safe. This was EB: choosing the lesser of two really bad options.
It was terrifying. But it was right.
Come back in two weeks for part two of this series, and I’ll tell you how and why. We don’t regret it, and neither does he. Not even a little.
***
Note: Epidermolysis Bullosa Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Epidermolysis Bullosa Today or its parent company, Bionews, and are intended to spark discussion about issues pertaining to epidermolysis bullosa.







Leave a comment
Fill in the required fields to post. Your email address will not be published.