Oral Surgery Becomes a Painful Nightmare for My Son
Written by |

My son Jonah, 12, had oral surgery on Dec. 22, which involved a simple extraction and some coating on his teeth to make them smoother. For most children, this probably wouldn’t have been a big deal. But for Jonah, who has epidermolysis bullosa (EB), the surgery was disastrous.
Jonah had to be intubated, which can be risky, but the anesthesia team did an amazing job. Imagine having to secure electrocardiogram leads, a pulse oximeter, and an oxygen mask without adhesives. Then imagine trying to place a tube down the trachea of a child with EB without causing damage.
Jonah’s throat did end up getting a couple of blisters, but overall, he was OK — from that part, anyway.

Jonah awaits oral surgery in a preoperative room on Dec. 22. (Photo by Patrice Williams)
During surgery, however, Jonah’s mouth was shredded. I don’t have photos because Jonah didn’t want me to take any. But believe me, it was awful. His lips were swollen and completely sheared of skin. He couldn’t even open his mouth enough to show me the inside of it, but about 90% of it was covered in raw lesions.
A poor pain management strategy
From the moment we began talking about the surgery, I had emphasized the need for good postoperative pain management that would last at least a week. On a normal day, Jonah has up to three lesions in his mouth, which prevent him from talking or eating. These can last up to three days. So, I knew the effects of surgery would be bad.
Yet doctors prescribed him just three days of Vicodin, because extraction patients typically don’t need more than that.
“Yes, but the extraction is not what I’m worried about,” I repeated over and over.
Extraction pain for Jonah would be about a level 4, because he is used to pain and his baseline for it is ridiculously high.
But a mouth ripped to pieces is more than he should have had to bear with only ibuprofen and a few days of Vicodin. But with the ongoing opioid crisis in the U.S., that’s all doctors would prescribe him.
When we got home, Jonah had a horrible reaction to the anesthesia and vomited for two days, which meant he couldn’t keep any pain medicine down. Doctors hadn’t prescribed him anything for nausea, so I had to call our pediatrician to ask for Zofran (ondansetron). Meanwhile, we were fighting to keep him hydrated (thank God for a G-tube and a friend who loaned us a feeding pump) and trying to avoid the ER, due to a spike in COVID-19 cases.
Complete agony
The experience was miserable and scary. On day three, Jonah finally was able to keep his food and medicine down, and we were able to alternate giving him ibuprofen and Vicodin. Still, he described his pain level as an 8.5. He cried a lot. He couldn’t smile, eat, talk, or brush his teeth. For eight days, he endured complete agony, and we were concerned that his wounds would become infected because he couldn’t brush or swish.
We tried Carafate (sucralfate), Maalox, and Benadryl, and baking soda swishes. All of them were agonizing, and nothing helped. There’s nothing worse than seeing your kid suffer like that and being powerless to help. It feels ruthless and cruel.
I ached to see Jonah smile and longed for him to be able to eat. And I really, really missed him.
A taste of recovery
Jonah is doing much better now. For each day he was in pain and couldn’t eat, he made a list of foods he would eat when he felt better. I told him he could choose one meal for each day that he wasn’t able to eat. So far, he’s had Little Caesars pizza, homemade chicken chili, his favorite wings from a local restaurant, and steak.
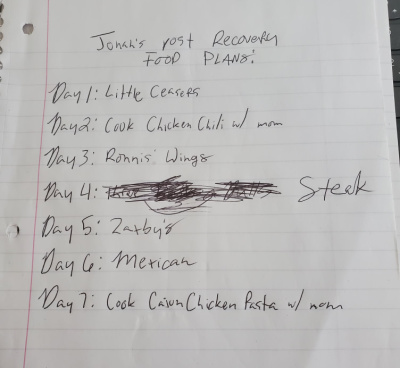
Jonah’s post-recovery food list he made during the week he couldn’t eat following painful oral surgery. (Photo by Patrice Williams)
I’m so glad he is doing better. But going through this experience was another unnecessary reminder that EB is a horrible disease. No child deserves this amount of suffering from such a supposedly “simple” procedure.
We have to find a cure.

Jonah finally enjoys food again after a traumatically painful surgery. (Photos by Patrice Williams)
***
Note: Epidermolysis Bullosa News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Epidermolysis Bullosa News or its parent company, Bionews, and are intended to spark discussion about issues pertaining to epidermolysis bullosa.







Leave a comment
Fill in the required fields to post. Your email address will not be published.