Plant-based Kaempferol May Help in Wound Healing in DEB: Cell Study
Written by |
Plant-based kaempferol — a compound with antioxidant and anti-inflammatory properties — enhanced the production in skin cells of C7, the protein that’s missing in people with dystrophic epidermolysis bullosa (DEB), a study demonstrated.
The findings suggest that kaempferol may provide therapeutic benefits to DEB patients. As such, the researchers noted that further evaluation of the compound’s effects on wound healing is needed.
“Kaempferol … could increase C7 production through multiple mechanisms due to its wide-ranging effects on cells including the reduction of inflammation, oxidative stress, DNA damage, fibrosis [scarring] and cancer development in a variety of different cell types,” the researchers wrote, adding that the compound “was found to help heal wounds in both rats and mice.”
Several other compounds that increased C7 also were found by genome-wide screening methods, which identified multiple genes and signaling pathways associated with DEB that can be investigated as potential therapeutic targets.
The study, “Genes and compounds that increase type VII collagen expression as potential treatments for dystrophic epidermolysis bullosa,” was published in the journal Experimental Dermatology.
DEB is caused by mutations in the COL7A1 gene, which provides instructions for a portion of the type VII collagen protein, known as C7, that helps connect and anchor different layers of the skin. These mutations lead to faulty or absent collagen, causing the skin to be fragile and easily torn, resulting in blisters and scar tissue.
There is no cure for DEB, and most management approaches try to prevent blisters — by protecting skin from injury — or treat them to avoid infections and further damage.
Identifying genes and/or small molecule compounds that increase the production of C7 may potentially restore the missing protein, improving skin strength and reducing damage. Such efforts could enhance quality of life for people living with DEB.
Genome-wide screening methods have been used to identify genes and pathways associated with therapeutic targets, including CRISPR activation (CRISPRa), which can selectively activate individual gene expression (activity).
Now, scientists at the University of Minnesota used CRISPRa to screen a library containing more than 18,000 genes to identify genes and pathways that trigger C7 production, and then screened candidate compounds shown to increase C7 protein.
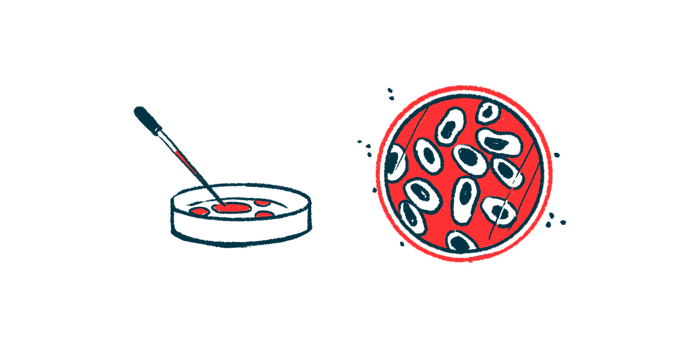
The team first developed a reporter cell line from keratinocytes — the primary type of cell found in the epidermis, the top layer of the skin. Cells were modified such that C7 expression was linked to a red fluorescent marker called tdTomato in a proportional manner. A red signal was generated when CRISPRa activated genes associated with C7 production.
The researchers then inserted the CRISPRa system and the gene library into C7_tdTomato cells. The screen identified two genes, DENND4B and TYROBP, as the most promising candidates. Selectively activating these genes, alongside COL7A1, increased the fluorescence, validating the screening results.
With DENND4B and TYROBP activation, there was no increase in the levels of COL7A1 messenger RNA, the molecule that carries the genetic instructions to make C7 protein, but rather a significant increase in C7 protein.
The gene DENND4B contains instructions for a protein potentially involved in transporting molecules across cell membranes, while TYROBP encodes for a protein that interacts with a variety of immune cell surface receptors to control cell activation.
The team then searched their list of candidate genes that increased C7, but to a lesser extent, for those that may interact with C7, DENND4B, and TYROBP proteins as part of a signaling pathway. Although only one protein was found to interact with DENND4B, multiple genes interacted with C7 or TYROBP.
“These results identified numerous signalling pathways and processes that could potentially be targeted to increase C7 production,” the researchers wrote.
Based on these findings, the team next conducted a targeted screen to identify small molecules that may enhance C7 production by various mechanisms, including increasing TYROBP. Initial screens identified multiple compounds that increased red fluorescence in C7_tdTomato cells.
Successful compounds were further evaluated in DEB skins cells that carry COL7A1 mutations as well as healthy skin cells.
The results showed that only kaempferol, found in plants, significantly increased both COL7A1 mRNA and C7 protein in DEB cells. In all other skin cell lines tested, DEB and normal, kaempferol enhanced C7 production.
These data suggested that “kaempferol could provide substantial therapeutic benefit to many individuals with DEB,” the investigators wrote. “Further development and testing of kaempferol as a therapeutic for wound healing and for DEB are necessary.”