Altered immunity discovered in study of adults with RDEB
Findings may aid in monitoring, classifying disease beyond 'skin injuries'
Written by |
Adults with recessive dystrophic epidermolysis bullosa (RDEB) have abnormal immune cell profiles in blood and skin samples, a study reveals. The patients also had high blood levels of pro-inflammatory fat-like lipids and immune signaling proteins.
These findings “underscore the concept of RDEB as [a] genetic disorder with distressed immunometabolism/inflammation,” the researchers wrote. “Our findings could be valuable for both clinicians and researchers, potentially laying the groundwork for a more tailored personalized monitoring and classification of RDEB beyond the skin injuries”
Details of the discovery were published in Nature Communications, in the study, “Systems immunology integrates the complex endotypes of recessive dystrophic epidermolysis bullosa.”
In RDEB, mutations in the COL7A1 gene disrupt the production of a portion of type VII collagen, a protein that connects the different layers of skin. When the protein is abnormal or missing, the skin becomes fragile and easily tears and blisters. The disease can also affect other body parts, including the mouth, eyes, digestive tract, and kidneys.
Studies have also discovered immune cell dysfunction in RDEB mouse models. Skin and blood analysis from RDEB patients suggests an abnormal abundance and activity of immune cells. Moreover, a recent study demonstrated that treatment with losartan, a commonly used blood pressure medication, reduced the signs of RDEB in children alongside a significant reduction in inflammatory markers.
“These observations bring into question the landscape of RDEB beyond skin and mucosa problems,” the researchers wrote.
Analyzing RDEB immunity
Here, a team led by researchers in France analyzed immune cells from people with RDEB who harbored different COL7A1 mutations and levels of disease severity, to further investigate the immunity of RDEB. Immune cells from age-matched healthy people served as controls.
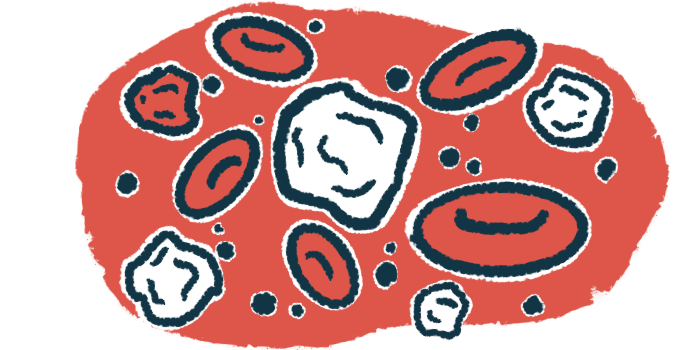
The analysis revealed substantial differences in immune cell populations in the blood of RDEB adults compared with healthy people. This included elevated levels of neutrophils and reduced basophils/eosinophils and monocytes. A less pronounced decrease in dendritic cells and lymphocytes, which includes T-cells, B-cells, and natural killer (NK) cells, was also observed.
When patient skin sections were compared with those from healthy controls, RDEB skin lesions were marked by neutrophils, B-cells, and plasma cells, which are white blood cells that arise from B-cells. Elevated numbers of activated CD4-positive and CD8-positive T-cells (also called cytotoxic T-cells), regulatory T-cells, monocytes, dendritic cells, and macrophages were also noted.
Looking more closely at lymphocytes, RDEB adults had an overabundance of effector CD4-positive T-cells, which are those required for executing immune functions. At the same time, there were lower numbers of naïve (immature) T-cells and regulatory T-cells, a subtype that helps maintain immune balance by suppressing inflammatory responses.
Likewise, there was an overabundance of cytotoxic T-cells compared with naïve cells, as well as defects in NK cells, which generally showed lower activity.
An analysis of the metabolic processes that drive T-cell and NK cell function found CD4-positive T-cells and, to a lesser extent, cytotoxic T-cells from RDEB patients had high metabolic activity, “supporting a potential activated/inflammatory [disease] state,” the researchers noted. The global metabolic activity of RDEB NK cells also differed from that of healthy controls.
Other inflammatory triggers
The researchers then examined fat-like lipids, some of which trigger inflammatory processes and have been linked to several chronic diseases.
Compared with controls, RDEB patient samples showed a significant decrease in the total amounts of neutral lipids like cholesterol and triacylglycerols, which are not linked to inflammation. In contrast, several eicosanoids, well-known lipid mediators of inflammation, were significantly altered in RDEB patients.
Similarly, the blood of RDEB patients has significantly higher levels of pro-inflammation immune signaling proteins called cytokines, which was “in line with the observed immunometabolic signature of RDEB adults and corroborates the current notion of systemic [bodywide] inflammation in RDEB,” the scientists wrote.
Lastly, the team constructed predictive models using machine learning, a type of artificial intelligence that uses programs to learn from data, and identify and predict patterns. Input data included cytokine levels, lipid profiles, and the number of circulating immune cells, collectively called the inflammation immunity score, or IIS.
The analysis separated RDEB adults into two distinct groups: moderate to high IIS and highest IIS. Those in the highest IIS group showed the most substantial increases in pro-inflammatory cytokines and lipid mediators, the output showed.
“Our findings underscore the necessity for further development of systemic strategies aimed at fine-tuning peripheral immune cell [balance] to lessen inflammation without compromising immune defense,” the researchers wrote. “Ultimately, this approach could lead to better management and improved quality of life for long-suffering RDEB adults.”