Blocking Notch signaling pathway could ease RDEB scarring: Study
Findings could 'set stage' for new urgently needed treatments, scientists say
Blocking the Notch signaling pathway — key to cell-to-cell communication — was found to significantly ease signs of fibrosis, or excessive scar tissue buildup, in skin cells from people with recessive dystrophic epidermolysis bullosa (RDEB) in a new study from Italy.
According to the researchers, Notch signaling was elevated in these patient cells, where it was associated with pro-fibrotic effects.
Such findings “could set the stage to design innovative therapeutic strategies to counteract RDEB-associated fibrosis and to offer RDEB patients a treatment they urgently need,” the team wrote.
The study, “Gamma-secretase inhibitors down-regulate the pro-fibrotic Notch signaling pathway in recessive dystrophic epidermolysis bullosa,” was published in the Journal of Investigative Dermatology.
Notch signaling pathway implicated in driving skin fibrosis
In RDEB, a lack of the connective tissue protein collagen type VII leads to fragile skin that easily blisters. Chronic skin wounds that are hard to heal are associated with inflammation and progressive fibrosis.
Such scarring not only is disabling, but it also contributes to the elevated risk of aggressive forms of skin cancer in these patients. No therapeutic approaches have been developed to date that can reverse RDEB-associated fibrosis.
“Fibrosis is, for the most part, diagnosed after it has progressed … making its treatment challenging and ineffective,” Alexander Nyström, PhD, and Jörn Dengjel, PhD, two scientists from Europe, wrote in a commentary accompanying the published study. Both are biology researchers not directly affiliated with the work.
The Notch signaling pathway is involved in a range of different biological processes — both healthy and disease-related ones — and has been implicated in driving skin fibrosis.
Previous research from the scientists in this study indicated that JAG1 and a form of NOTCH1, two Notch proteins, are increased in cells from RDEB patients compared with healthy people, and also are correlated with other pro-fibrotic molecules.
Now, the team further explored the possible role of the Notch pathway in RDEB, and whether its inhibition — meaning, blocking it — might have therapeutic effects.
As in their previous study, JAG1 and NOTCH1 were elevated in RDEB skin fibroblasts, a type of connective tissue cell, compared with those of healthy people. Levels of Notch-associated proteins were further increased upon exposure to TGF-beta1, a molecule known to contribute to RDEB-associated fibrosis.
That finding suggests that TGF-beta1 might help to trigger or sustain Notch signaling in RDEB, according to the researchers. Likewise, evidence suggested that reductions in autophagy — the process by which cells recycle old, damaged, or unneeded cellular components — also might promote Notch signaling.
Treatment seen to counteract pro-fibrotic effects in cells
To investigate the possible effects of Notch inhibition in RDEB, the scientists treated the cells with DAPT or PF-03084014, also known as nirogacestat. Both of these molecules are inhibitors of gamma-secretases, a family of enzymes needed for Notch signaling to occur.
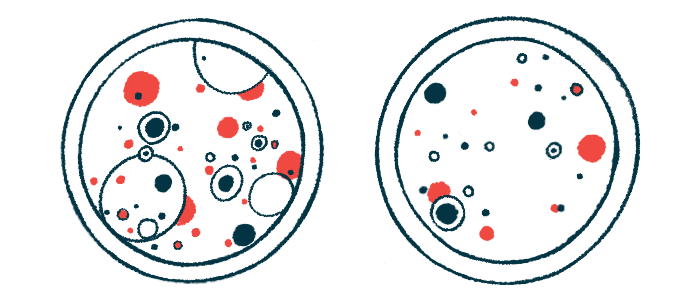
These treatments counteracted many of the pro-fibrotic effects that are observed in RDEB cells.
During wound healing, fibroblasts activate and convert to myofibroblasts, which have strong contractile abilities to help close wounds and release pro-fibrotic markers. However, their excessive growth and activity also is associated with harmful fibrosis.
PF-03084014 was associated with significant reductions in fibroblast contractility, and blocked fibroblast growth, movement, and expression of pro-fibrotic markers, all of which are indicators of their activation.
The treatment also linked to diminished levels of TGF-beta1 and a reduced secretion of collagen, the protein that helps form scar tissue.
DAPT treatment was associated with similar, but less substantial therapeutic effects.
The findings position these gamma-secretase inhibitors as possible therapeutic targets for RDEB fibrosis. However, there are several necessary avenues for future study — including evaluating the molecules in animal models of RDEB.
Although PF-03084014 generally was found to be more effective than DAPT, Nyström and Dengjel emphasize it will still be important to include DAPT in these studies, as the behavior of these medications might be different in live animals then cells in a lab.
Emerging and recently approved gene therapies, including Vyjuvek — a U.S.-approved gene therapy gel — are changing the RDEB treatment landscape, according to researchers.
It is possible that therapies like gamma-secretase inhibitors might eventually serve as symptomatic relief when used in conjunction with such treatments. It will thus be important, the team noted, to ensure there are no harmful effects of combining them.
Also importantly, it will be critical in future research “to carefully determine potential adverse events of long-term use because these drugs would need to be given continuously throughout life to protect against fibrosis,” Nyström and Dengjel wrote.