IV Immunoglobulin May Help Treat Inflammation in Severe EBP, Case Report Suggests
Written by |
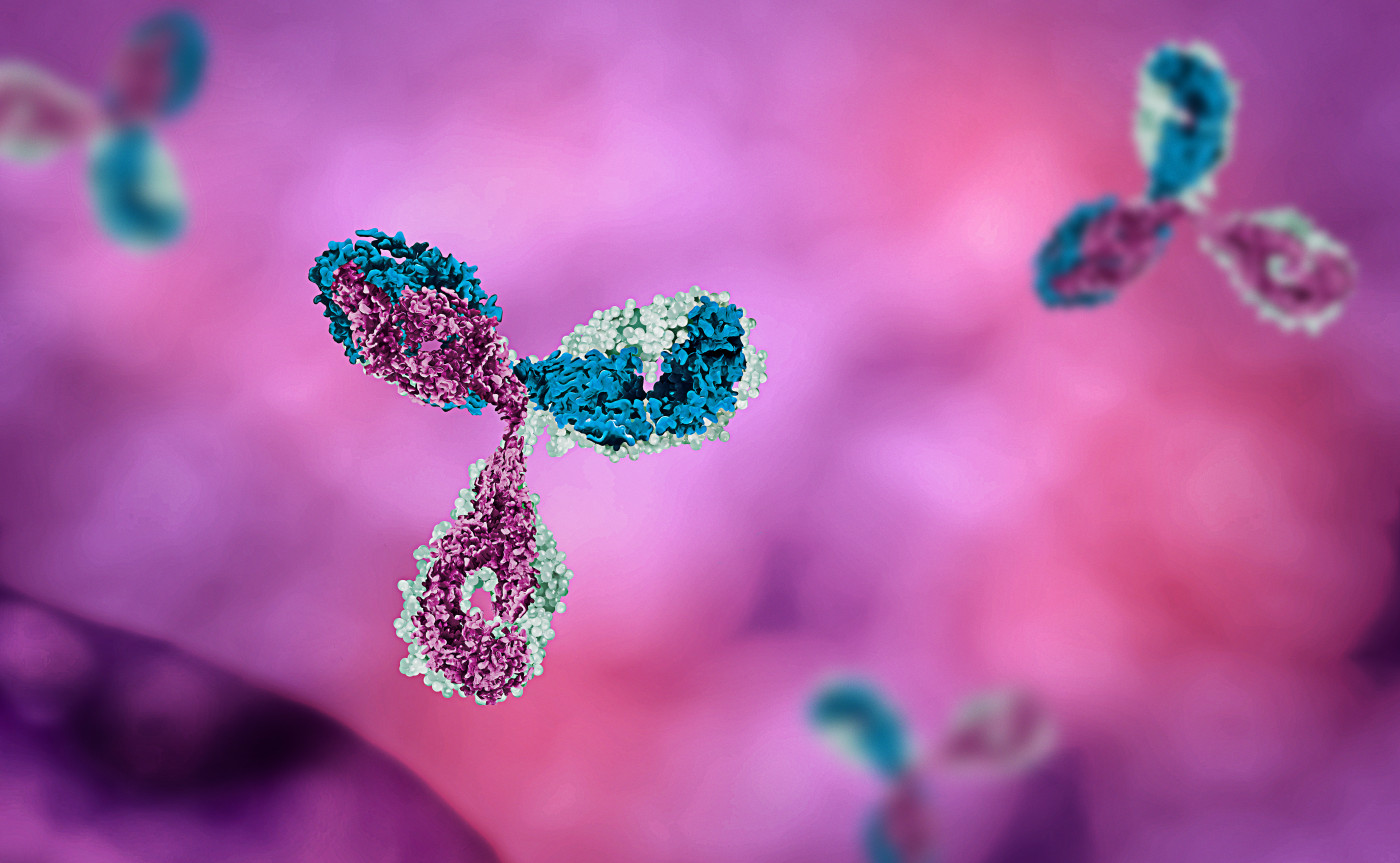
Intravenous immunoglobulin (IVIG) may be a promising treatment for reducing inflammation in severe epidermolysis bullosa pruriginosa (EBP) — a rare type of dystrophic epidermolysis bullosa (DEB) marked by severe itching of the skin — that fails to respond to other therapies, a case report suggests.
A 43-year-old woman in Turkey saw a substantial reduction in her skin lesions and itching following such treatment, in which blood plasma containing immunoglobulins was administered intravenously (into the vein).
The study, “Promising effect of intravenous immunoglobulin therapy for epidermolysis bullosa pruriginosa,” was published in the International Journal of Dermatology.
In addition to the blisters, skin lesions, and abnormal fingernails that are common in DEB, people with EBP also experience intense itching, which can significantly worsen their other skin problems.
Such symptoms usually begin in the first years of life, but a diagnosis is often hindered by overlapping symptoms with other inflammatory skin disorders. While treatments mostly focus on reducing inflammation and easing itching, they have limited efficacy. In addition, treatment strategies are not well established.
Here, a team of researchers from Turkey outlined the case of a woman with severe EBP who was successfully treated with IVIG therapy after failing high-dose steroids and the immunosuppressant cyclosporine.
IVIG is a form of therapy in which patients are given a pool of antibodies (immunoglobulins) derived from the blood plasma of healthy donors. The treatment was originally developed as a form of antibody replacement therapy to prevent serious infections in people with compromised immune systems. Researchers later showed it also can be used to neutralize harmful immune responses in individuals with autoimmune conditions.
This woman sought treatment from a dermatology clinic for skin erosions and blisters all over her body, along with severe itching. Her symptoms had been present since her first year of life, but the disease was still undiagnosed.
Six other members of her family, ages 11 to 75, shared similar symptoms. All had experienced complications since infancy and all were found to have the same mutation in the COL7A1 gene. That gene provides instructions for making a protein used to ultimately assemble a larger protein called type VII collagen. The mutation, termed c.6127G>A, is the most common COL7A1 mutation identified in dominant DEB patients, highlighting that no specific mutations in this gene define EBP.
All of the patients had abnormalities in the toenails, and some also had problems in the fingernails, as well as small skin bumps (milia), skin eruptions, and excoriations — caused by excessive scratching — which led to a diagnosis of EBP.
High immunoglobulin E (IgE) levels in circulation — the antibodies produced in allergic reactions — were found in six patients, though none had a higher propensity for allergic diseases.
The three women had more severe disease than the men, the researchers noted. The symptoms also tended to get worse during pregnancy, indicating that “hormonal factors may have a crucial role in inflammation seen in EBP and may explain [clinical] variability in some families,” they wrote.
The initial patient, whose disease was analyzed in greater detail, had the most severe symptoms. Specifically, 76.6% of her skin was affected by the disease — as compared with 2.7% to 44.1% among other family members. She was first treated with high-dose steroids, and later with steroids and cyclosporine for two years. However, her disease activity was not reduced to a satisfactory level.
The woman was then offered monthly 2 g/kg IVIG therapy for one year. After six months on this treatment, skin lesions severity and itching had reduced substantially. The amount of immune cells called eosinophils in skin lesions also was lowered. But within three months of stopping IVIG, the woman experienced symptom worsening, and IVIG treatment was restarted.
“Treatment of EBP is difficult, as evidenced by a large number of anecdotal reports of treatments, most of which have only been partially effective,” the researchers wrote.
But the findings support immunoglobulin treatment as “a promising therapeutic approach to antagonize immune cell infiltration and patient symptoms in EBP,” particularly in severe cases that fail to respond to other therapies, they added.