Gene-editing therapy corrects LAMB3 mutation in JEB skin cells
Scientists project new approach could be used in other EB genetic causes
Written by |
A gene-editing therapy made to correct a genetic defect in the LAMB3 gene that’s known to cause junctional epidermolysis bullosa (JEB) worked as intended and restored more normal laminin 332 protein levels in skin cells from a JEB patient.
To make the treatment more precise and safer, the scientists utilized newer gene-editing tools that are less likely to cause unintended DNA damage. This approach could eventually be used to treat JEB patients with LAMB3 mutations and could also be modified to address other genetic causes of epidermolysis bullosa (EB), the scientists said.
“This protocol represents a significant improvement in precision gene repair … with the potential to be applied to a large cohort of patients harboring this prevalent [disease-causing] variant, as well as other forms of EB,” they wrote. The study, “Efficient dual Cas9 nickase correction of a prevalent pathogenic LAMB3 variant for junctional epidermolysis bullosa,” was published in JID Innovations.
JEB is a form of EB that’s most often caused by mutations in one of three genes — LAMA3, LAMB3, or LAMC2 — that together encode the production of laminin 332. About 70% of cases are caused by LAMB3 mutations.
Laminin 332 is important for holding skin layers together. It’s part of the basement membrane, a matrix of proteins that provides skin with structural support. Disruptions in its production or function in JEB lead to skin that easily tears and blisters. This can also drive other complications, such as infections and an increased risk of skin cancer.
Gene therapies for treating EB, JEB
Gene therapies are of interest for treating forms of EB, including JEB. The most commonly tested approach so far is gene replacement therapy, wherein a new and healthy version of a gene is provided to replace a faulty one.
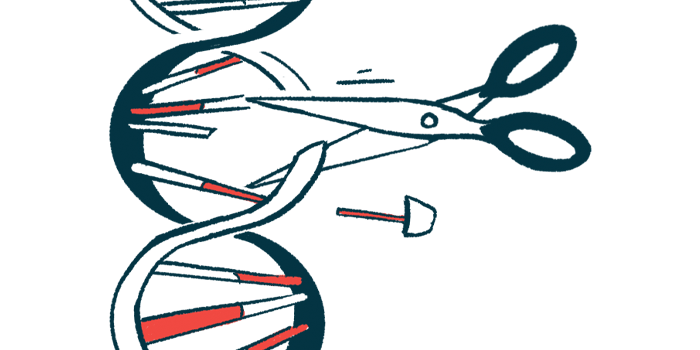
Gene-editing approaches involve correcting the genetic defect in a person’s own gene. This can be done with genome-editing technologies such as CRISPR/Cas9, which function as a kind of molecular scissors for cutting and editing DNA.
A possible drawback of gene-editing therapies is that they can lead to unintended DNA damage, called genotoxicity. Scientists have been working on creating better gene-editing strategies to help minimize that and improve their safety.
Here, the researchers developed a gene-editing therapy to correct the most common JEB-causing mutation in LAMB3, called c.1903 C > T. It used special enzymes called Cas9 nickases that should lead to less genotoxicity than the standard CRISPR/Cas9 editing system.
The scientists found their gene-editing therapy was able to correct the genetic defect without signs of off-target DNA editing in skin cells taken from a JEB patient.
While there was very little secretion of laminin 332 from uncorrected cells, the gene-edited cells exhibited increased secretion of the protein to around 30% of normal. Accordingly, the cells’ ability to attach to the dish they were grown in was also increased, consistent with laminin 332’s role in helping skin cells adhere to each other.
The scientists also tested their approach in a three-dimensional skin model developed from the patient’s skin cells. Again, the gene correction led to a more normal expression of laminin 332 between skin layers. This was accompanied by an increased thickness of the epidermal layer, the outermost layer of skin. The epidermis is normally thinner than usual in JEB, likely due to defective laminin 332 signaling. An increase in Np63-alpha, a protein involved in skin cell growth and survival, was also observed in the gene-corrected skin.
“These data … potentially open the door for therapeutic gene editing facilitated by Cas9 nickases,” the researchers wrote. “Given the simplicity and cost-effectiveness of this protocol, it has the potential to be tailored to address other pathogenic EB variants.”