Mix of treatments may aid survival in RDEB patients with skin cancer
Treatments after skin cancer surgery found to extend patient survival: Review
Written by |
Additional treatments following surgery for squamous cell carcinoma (SCC), a type of skin cancer, may prolong survival in people with recessive dystrophic epidermolysis bullosa (RDEB), according to a review study.
“However, it is difficult to attribute extended survival to any single treatment, as multiple therapeutic modalities are often used to treat [RDEB-SCC],” researchers wrote.
The study, “Therapies for cutaneous squamous cell carcinoma in recessive dystrophic epidermolysis bullosa: a systematic review of 157 cases,” was published in the Orphanet Journal of Rare Diseases.
DEB is caused by mutations in the COL7A1 gene, which encodes for a portion of the type VII collagen protein, which connects different layers of the skin. When collagen is faulty or missing, skin connections are fragile, and even small movements can cause the layers to separate and lead to blisters and scar tissue formation.
Squamous cell carcinoma is a leading cause of death in RDEB
Patients must inherit two copies of disease-causing mutations, one from each parent, to develop RDEB, in which SCC is a leading cause of death. However, health outcomes of people with RDEB-SCC have mainly been described in case reports.
The surgical removal of the affected skin areas is the first line of treatment for RDEB-SCC. Other therapies may also be recommended for advanced cancer, including chemotherapy, radiotherapy, immunotherapy, and anti-epidermal growth factor receptor (EGFR) antibodies.
To summarize clinical advancements, researchers in the U.S. conducted a review of RDEB-SCC patient outcomes. A total of 157 studies were identified from online databases and included in the analysis.
The median age at diagnosis, specified in 144 patients with both RDEB and SCC, was 30 years. Seven patients were younger than 18. In most cases, the cancer was well-differentiated, which means less aggressive tumors (64.1%), wound-related (59.6%), and at least 2 centimeters in size (77.6%).
Skin lesions were most often present in the feet, shins, hands, and forearms. Overall, 41 patients had metastatic lesions closer to the main lesion, while eight had more distant cancer spread.
Surgery, most commonly the removal of the skin lesion or limb amputation, was the primary form of treatment. After surgical removal, performed in 96 patients, nine developed metastases. A similar outcome was found in three of 29 patients who underwent amputations. Three more achieved complete cancer remission, and five died.
Results of electrochemotherapy were more favorable
Thirty patients underwent chemotherapy: 12 conventional chemotherapy medications and 18 electrochemotherapy, which is a technique that uses electric pulses to send the chemotherapy into cancer cells. In comparison, the results of electrochemotherapy were more favorable, with disease progression experienced by two of 13 patients whose outcome was described.
“These results further support existing recommendations that electrochemotherapy may be a potential treatment for [RDEB-SCCs],” the scientists wrote.
A total of 24 patients received radiotherapy, while two received topical photodynamic therapy, a treatment that kills cancer cells by combining light energy with a drug.
The anti-EGFR therapy cetuximab was used in 13 patients, with some cases of tumor progression or recurrence after initial improvements being reported. Eleven patients received immunotherapies, most frequently Libtayo (cemiplimab), with two patients experiencing complete response to treatment.
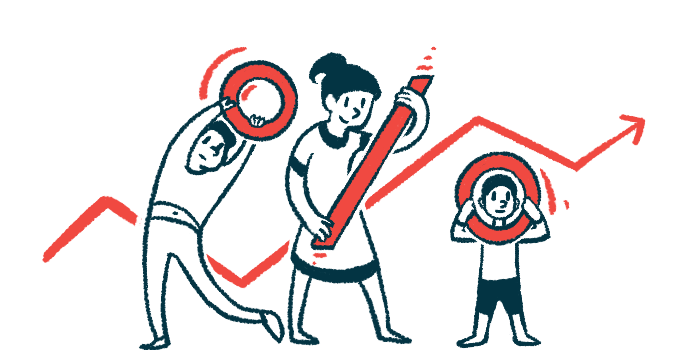
Considering the aggressive nature of RDEB-SCC, successive treatments are often used, making it difficult to determine the exact benefits of each therapy. However, in most cases, the study found that additional treatments after surgery prolonged patient survival.
Median survival time was highest with surgery, chemotherapy, radiotherapy
The median survival time was the highest — 9.5 years — in patients who underwent surgery together with chemotherapy and radiotherapy, followed by surgery plus immunotherapy (4.6 years), and surgery with radiotherapy or with anti-EGFR therapy (four years in both cases). The lowest survival was with surgery alone (two years) and with surgery and chemotherapy (1.85 years).
Treatment-related side effects were mainly limited to impaired wound healing, reported in patients treated with immunotherapies, and nausea and fatigue for those receiving anti-EGFR therapies.
“Despite the challenges of a limited sample size in a rare disease,” the researchers wrote, “this systematic review provides an overview of treatment options for [SCC] in RDEB.”