Non-viral gene-editing strategy may be promising way to treat RDEB
Approach needs more testing in patient cells and animal models, researchers say
Written by |
A new gene-editing strategy that does not require the use of a virus can effectively correct a COL7A1 gene mutation in skin cells derived from people with recessive dystrophic epidermolysis bullosa (RDEB), according to a recent report.
Most gene therapies in development require the use of viral carriers to help them get into human cells, but this can pose certain safety risks.
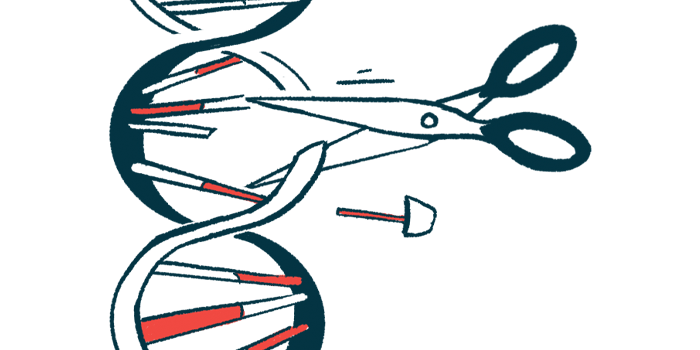
The strategy tested in the study instead used non-viral carriers to deliver a therapy that would delete a protein-coding stretch, or exon, of COL7A1 called exon 80, where the mutation is found in RDEB patients.
“The … approach developed here has great potential to be used as a topical treatment for RDEB patients with mutations in COL7A1 exon 80,” researchers wrote. “Besides, this therapeutic strategy can easily be adapted for mutations in other COL7A1 exons, other epidermolysis bullosa subtypes and other genetic diseases.”
The study, “CRISPR/Cas9 Based Non-viral Gene Editing Therapy for Topical Treatment of Recessive Dystrophic Epidermolysis Bullosa,” was published in Molecular Therapy – Methods & Clinical Development.
RDEB caused by mutations in COL7A1 gene
In RDEB, mutations in COL7A1 lead to a lack of production of functional type VII collagen, or C7, a connective tissue protein that helps anchor skin layers together. As such, patients have skin that easily tears and blisters.
Gene therapies to correct the mutation or replace the problematic gene altogether are of significant interest for treating the disease.
Earlier this year, a gene therapy called Vyjuvek (beremagene geperpavec) was approved in the U.S. Given as a gel directly onto skin wounds, Vyjuvek delivers to skin cells a functional version of COL7A1, packaged into a modified version of the herpes virus.
Gene-editing approaches, instead of replacing the gene, would deliver to cells the tools needed to correct or remove the mutation in the existing gene. A commonly used gene-editing tool is called the CRISPR-Cas9 system, which is derived from the natural defense mechanisms found in bacteria.
The viral carriers used for gene-editing therapies are intended to help them be taken up more easily by cells — viruses are highly adept at entering human cells.
…this therapeutic strategy can easily be adapted for mutations in other COL7A1 exons, other epidermolysis bullosa subtypes and other genetic diseases.
Safety concerns with viral gene-editing therapies
While these viral carriers are modified so as not to cause disease, their use still has certain safety drawbacks, such as the possibility of causing an immune reaction in the recipient, cancer, or DNA damage, according to the researchers.
They also typically require a lengthy process involving obtaining cells, editing them in the lab, then transplanting them back into the skin.
Using a non-viral carrier could have certain advantages, in terms of safety, capacity for therapeutic cargo, and cheaper and easier manufacturing.
In their study, the scientists set out to develop a non-viral approach for deleting exon 80, the site of a known RDEB-causing mutation called c.6527dupC common among Spanish patients.
A virus-based strategy for deleting exon 80 was previously found to effectively restore type VII collagen production in mice.
Moreover, a non-viral approach called electroporation was able to successfully delete exon 80. However, this uses a high electrical voltage to insert the therapy directly into cells, and may be less feasible when considering direct application to patient skin.
To overcome these limitations, the team packaged a gene-editing therapy to delete exon 80 into a new type of non-viral carrier called highly branched poly(beta amino 18 ester)s, or HPAEs.
New gene-editing therapy did not show signs of toxicity
In skin cells derived from RDEB patients with that mutation, the new gene-editing therapy was efficiently taken up by the cells, and importantly, did not show signs of toxicity.
Data also indicated the therapy led to successful deletion of exon 80. The therapy also restored C7 production, reaching about 29% of levels seen in healthy cells. While this number may seem low, research has indicated that 10% of C7 protein was sufficient to reduce blistering and lower disease severity in RDEB, the scientists noted.
In future work, this new non-viral approach should be tested further in patient cells and animal models, the scientists added.
Moreover, “to facilitate the clinical translation, it is imperative to further formulate the HPAEs and gene material nanoparticles into a topical medicine,” they wrote.
Topical application, such as that used with Vyjuvek, makes it easier to deliver the treatment during routine wound dressing, “minimizing any additional trauma and maximizing convenience to patients,” they noted.