Treatments focused on wound healing may be beneficial in severe EB
Study probes vicious cycle of inflammation in the healing process

Issues with wound healing may play a central role in driving severe forms of epidermolysis bullosa (EB), a new paper proposes.
Scientists think that, in EB, wounds may enter a vicious cycle where they become inflamed as they try to heal, but then are unable to resolve the healing process, ultimately triggering more inflammation that leads to tissue damage and blistering.
Based on this idea, the researchers propose that “approaches that modulate inflammation and accelerate wound healing could be clinically meaningful and potentially benefit patients and their caregivers.”
Their study, “Mapping the burden of severe forms of epidermolysis bullosa – Implications for patient management,” was published in the journal JAAD International. The work was funded by Amryt Pharma, which markets the EB treatment Filsuvez (Oleogel-S10).
Junctional EB (JEB) and dystrophic EB (DEB) are the two most severe forms of EB. These disorders are caused by mutations in genes that are important for making the body’s connective tissue, and characterized by symptoms such as widespread blistering and scarring.
The precise biological mechanisms that lead to health problems for people with JEB or DEB remain incompletely understood. Better understanding of the biological underpinnings of the disease may open new doors toward developing novel therapies.
Here, a team of scientists set out to identify potential mechanisms that could contribute to disease in JEB or DEB using a type of analysis called burden mapping, which involves a review of available data from the scientific literature combined with interviews with experts in the field.
“Despite inherent issues of subjectivity, this approach shows promise in consolidating and corroborating heterogenous [variable] evidence to generate hypotheses on the clinical relevance of underlying disease mechanisms in rare diseases,” the researchers wrote.
Results showed that most disease manifestations of JEB and DEB affected patients’ skin, though other bodily systems — including the heart, digestive tract, lungs, kidneys, and visual system — also could be affected, mainly due to blistering in nearby tissue. The burden mapping analysis suggested, in particular, a defect in wound healing.
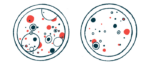
When the body is wounded, it normally goes through a three-step process to heal: first, the wound becomes inflamed, allowing the immune system to remove damaged cells and destroy any infectious invaders. After the inflammation resolves new cells are grown — a process called regeneration —before the healed tissue fully matures.
In JEB and DEB however, mutations impair the normal healing process, and wounds end up getting stuck in the inflammation stage. That sets off a vicious cycle in which inflammation causes more damage to tissues and prevents regeneration of the epithelial cell layer, subsequent blistering and wounding make infections more likely, and itching sets off an itch-scratch-blister cycle.
“Our findings propose a role for delayed wound healing in the burden of severe forms of EB – predominantly mediated through inflammation,” the researchers concluded.
The team stressed that this analysis was designed to generate hypotheses for future study, so more work will be needed now to test these ideas.