Fibroblast Skin Injections Show Promise in Healing Wounds in Dystrophic Epidermolysis Bullosa Patients, Study Finds
Injecting fibroblasts directly into a wound led to higher rates of healing and complete closure than other more common methods in patients with recessive dystrophic epidermolysis bullosa (RDEB), a severe form of epidermolysis bullosa, researchers found.
Findings were reported in the study, “Cultured allogeneic fibroblast injection versus fibroblasts cultured on amniotic membrane scaffold for dystrophic epidermolysis bullosa treatment,” published in the British Journal of Dermatology.
In the study, researchers compared different methods of healing wounds based on fibroblasts in patients with RDEB.
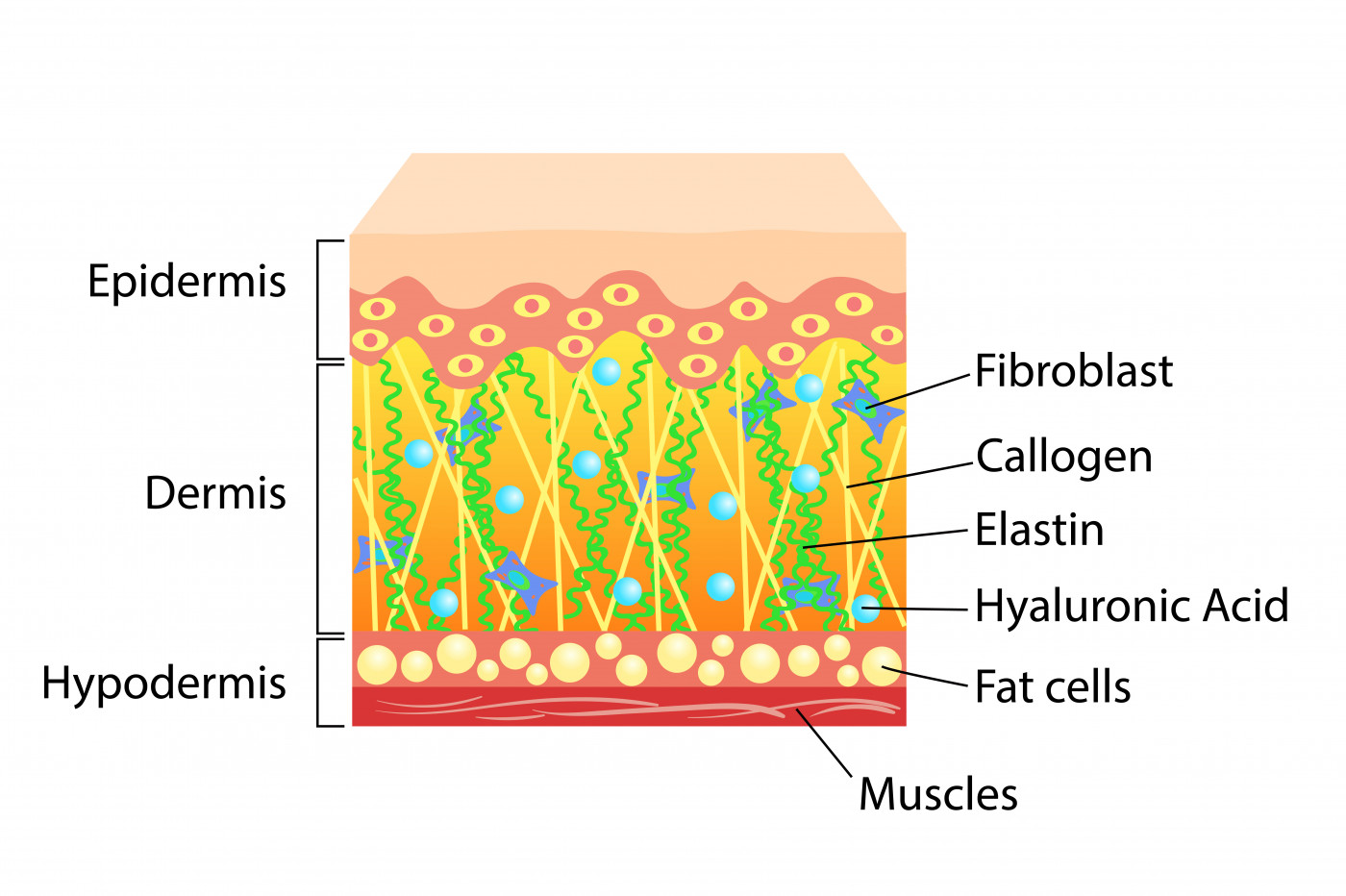
Fibroblasts are the major cells producing collagen. Researchers obtained the cells used in the study from the foreskin of a genetically healthy male infant. The cells were then grown in culture before being administered by injection into the wound site. This technique is referred to as intradermal injection of cultured allogeneic fibroblasts.
The team compared this technique with one using fibroblasts seeded on an amniotic membrane scaffold (FAMS) before being added to a wound, and standard treatment with Vaseline gauze.
Previous studies showed that “only the amniotic membrane has been successfully used in dressing and promoting closure of EB [epidermolysis bullosa] wounds,” the researchers wrote. However, the healing potential of fibroblasts seeded on amniotic membranes has never been tested in RDEB wounds.
Results showed that after two and 12 weeks after treatment, the size of the wounds treated with fibroblast injections and FAMS had significantly decreased compared with control wounds.
Better results were seen with intradermal injection of fibroblasts than with FAMS. Injecting fibroblasts resulted in a complete closure of 66.6% of the wounds, compared with only 4.7% of the wounds treated with FAMS.
The ability to induce the formation of a continuous layer of collagen was the key factor for complete wound healing, the researchers said. This was achieved in wounds treated with fibroblast injections “but was not continuous or complete in lesions treated with FAMS,” they said, supporting the superiority of fibroblast injections over FAMS.
Because wound healing in patients with RDEB is a challenge, the results suggest that intradermal injection of fibroblasts is a potentially effective treatment strategy for these patients.
“Although culturing fibroblasts is an expensive and arduous task, the injection is a simple procedure that can be performed in the outpatient setting, providing improved healing of chronic wounds,” the team concluded.






