Collagen VII Protein Important in Immune Response to Bacteria in EB, Mouse Study Shows
Written by |
The systemic administration of collagen VII protein can reduce bacteria in the skin of mice with epidermolysis bullosa (EB), according to a report published in the journal Proceedings of the National Academy of Sciences.
The study, “Impaired lymphoid extracellular matrix impedes antibacterial immunity in epidermolysis bullosa,” showed that collagen VII is required in the spleen to support the activity of immune cells and promote their innate defense mechanisms.
This finding may help researchers understand why people with epidermolysis bullosa, a rare genetic disease caused by a mutation in the COL7A1 gene — which provides instructions for the protein collagen VII — are more susceptible to developing wound infections. The results may also open new therapeutic avenues to treat EB.
For many years, collagen VII has been considered a skin-specialized protein, as it is the main structural element that ensures skin’s integrity. But this protein isn’t restricted to the skin and can be found in other places in the body.
The role of collagen VII in these other tissues has not been fully understood.
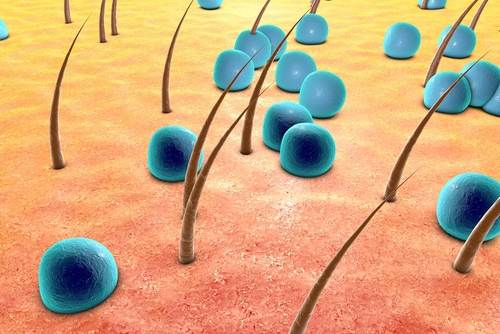
People with EB who lack collagen VII have fragile skin that can easily form blisters and wounds. They are also highly susceptible to increased bacterial colonization of the skin, which can lead to infection of the skin wounds.
Based on the characteristic symptoms of these patients, a research team at the University of Fribourg in Germany wondered if collagen VII could be involved in the mechanisms of immune defense.
So researchers started by comparing mice with EB to healthy mice. They found that the diseased animals had increased bacteria in the skin, regardless of whether they had skin wounds.
Also, collagen VII protein was found in the spleens of healthy mice, while it was nearly absent in the spleens of mice with epidermolysis bullosa.
Interestingly, the researchers found that collagen VII was interacting with cochlin — a protein required for the activation of immune cells — and sequestered it inside the spleen.
Additional experiments revealed that, in the absence of collagen VII, cochlin protein was not retained in the spleen, resulting in an increased bacterial burden in the skin.
When researchers injected collagen VII protein in mice with EB, the levels of the protein were restored in the spleen (but not in the skin), resulting in the reactivation of innate immune cells and a reduction in bacterial skin colonization.
“Taken together, our study promotes a shift of the view of RDEB [recessive dystrophic epidermolysis bullosa] as a mucocutaneous blistering disorder to a systemic disease with multi-organ involvement,” the researchers wrote.
The study shows that collagen VII plays a unique role in the systemic defense against bacteria, which may pave the way for new therapies that target the collagen VII-cochlin axis, the team suggested.