Gene editing increases type VII collagen production in skin cells
Study used lab-grown cells from the skin of 2 people with recessive DEB
A gene editing strategy corrected a disease-causing mutation in lab-grown cells derived from the skin of two individuals with recessive dystrophic epidermolysis bullosa (DEB), according to a study by researchers in the U.S. and France.
“With this promising non-viral approach, we achieved therapeutically relevant specific gene editing,” the researchers wrote. As a result, production of type VII collagen, which is missing in recessive DEB, increased to more than half the levels seen in healthy skin cells.
The study, “Highly efficient ex-vivo correction of COL7A1 through RNP-based CRISPR/Cas9 and Homology-Directed Repair to treat recessive dystrophic epidermolysis bullosa,” was published in the Journal of Investigative Dermatology.
DEB is caused by mutations in the COL7A1 gene, which provides instructions for making part of a protein called type VII collagen. This protein forms rope-like structures that hold the different layers of skin together.
When type VII collagen is missing, the skin becomes very fragile and blisters or tears easily. People with the recessive form of DEB must have inherited two copies of the mutated gene, one from each parent, to develop symptoms.
Now, researchers tested the use of CRISPR/Cas9 to edit a disease-causing mutation in keratinocytes — the cells that produce keratin, a protein that makes up skin, hair, and nails — and fibroblasts (the cells that produce collagen) derived from two individuals with recessive DEB.
The approach uses a specially designed RNA molecule to guide an enzyme called Cas9 to a specific point in a DNA sequence. The enzyme cuts open the DNA at that point to remove, alter, or add DNA.
The researchers experimented with three different guiding RNA molecules. After getting delivered into the lab-grown keranocytes and fibroblasts, one of the guiding RNA molecules had a cutting accuracy of about 73% in both types of cells.
When the researchers delivered this guiding RNA molecule together with a piece of genetic material containing a blueprint to correct the disease-causing mutation, called c.6508C>T, more than half of the cells now had edited gene copies.
Gene editing led to increased production of type VII collagen
Left untreated, keranocytes and fibroblasts derived from the two individuals with recessive DEB did not produce any type VII collagen. Gene editing, however, increased production of type VII collagen to up to 56% the levels seen in healthy skin cells.
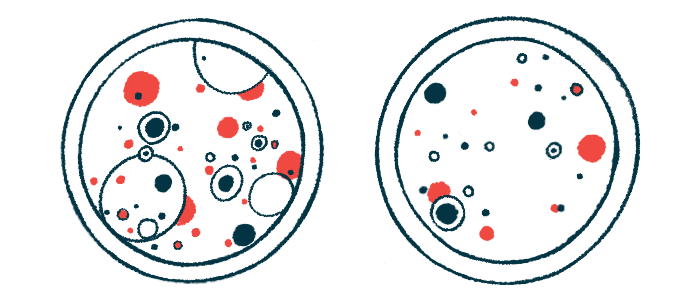
The lab-grown cells were used to grow three-dimensional models that closely mimic the structure and function of human skin, and then grafted onto mice to watch for production of type VII collagen.
In the presence of the disease-causing mutation in the COL7A1 gene, skin tissue lacked type VII collagen and the anchoring cord-like fibers that bind the epidermis (the outermost layer of skin) and dermis (an inner layer) together.
Treatment with CRISPR/Cas9 not only restored the production of type VII collagen at the interface between the epidermis and dermis, but also allowed anchoring points to form. These anchoring points were “thick, with cross-binding characteristic structure,” the researchers wrote.
While more research is needed to confirm its ability to correct other disease-causing mutations in the COL7A1 gene, “this approach has a potential for future ex-vivo [outside of the living body] clinical applications,” the researchers concluded.







