JEB Involving Kidneys, Lungs Should be Classified as Mixed Form of Disease, Case Report Suggests
Written by |
A case report of a patient with mild junctional epidermolysis bullosa (JEB) with kidney and lung involvement who showed blisters on different skin layers suggests that this type of epidermolysis bullosa (EB) should be classified as mixed instead of junctional.
The study, “A Nonjunctional, Nonsyndromic Case of Junctional Epidermolysis Bullosa With Renal and Respiratory Involvement,” was published in the Journal of the American Medical Association-Dermatology.
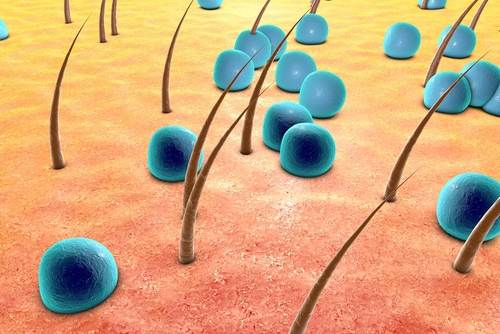
Epidermolysis bullosa groups various genetic conditions that cause tearing and blistering of the skin. The types of EB are classified based on which layers of the skin have blisters. Mixed forms of the disease typically involve more than one skin layer.
In JEB, the affected layer is the lamina lucida, a component of the basement membrane, which separates the epidermis (upper layer of the skin) from the dermis (lower layer of the skin). Severe cases of this condition can affect internal organs such as the digestive tract.
Researchers in Israel reported the case of a male patient in his late teens with a mild form of JEB with renal and respiratory involvement who only exhibited symptoms in the skin and mucosa.
The patient went to the hospital with misshapen and damaged toenails, joined toes, and obstruction of the tear duct. He first exhibited symptoms at 2 years old when he lost his eyebrows and eyelashes.
When he was 12, he had blisters on his shins that healed, causing redness and milia (small cysts) in the skin. He had reoccurring difficulties urinating due to obstruction of the urethra and had to undergo various surgeries for this issue.
He did not report any systemic symptoms, and his blood and urine exams, as well as pulmonary function, were normal.
Genetic analysis showed that the patient had mutations in both copies of the ITGA3 gene, which holds the instructions to produce integrin α3, a protein essential in the formation of the epidermis, kidneys, and lungs.
Further investigation showed he had low levels of integrin α3, but he produced normal amounts of other molecules integral for skin formation such as integrin β1 and collagen XVII.
Cases of JEB due to mutations in the ITGA3 gene are rare, with only eight cases reported so far. Other patients with these mutations had fused fingers and toes and manifestations in the kidneys and lungs.
Six out of these eight patients died at an early age due to renal and/or pulmonary disease.
“To our knowledge, the present case represents a unique form of junctional EB-RR [JEB with renal and respiratory involvement] manifesting only in the skin and mucosa. The mild phenotype is probably due to residual expression of integrin α3 compared with its total absence in previously reported cases,” the researchers said.
The doctors performed a skin biopsy of the blisters and observed them under the electron microscope. These examinations revealed that the patient had blisters in the lamina densa — a component of the basement membrane — and a discontinuous basement membrane.
A case report of another patient with mutations in the ITGA3 gene also described blisters in different components in the basement membrane, not exclusively in the lamina lucida as is the case in JEB.
“Therefore, junctional EB-RR may be better classified away from the functional group into a ‘mixed group’ together with Kindler syndrome,” the investigators concluded.





