Next-generation DNA Sequencing Efficiently Identifies Novel Mutation Causing Junctional EB in Newborn
Next-generation sequencing — a technique that reads DNA sequences much faster and cheaper than standard approaches — successfully identified a novel mutation in the LAMB3 gene in a newborn with junctional epidermolysis bullosa (EB), a case study reports.
The study, “Targeted next-generation sequencing identifies a novel mutation of LAMB3 in a Chinese neonatal patient presented with junctional epidermolysis bullosa,” was published in the journal Medicine.
EB is a group of disorders collectively characterized by skin fragility and blistering. While several disease-causing mutations have been well-documented, new mutations linked to EB are still being identified.
Because of the overlap of symptoms among different EB subtypes, being able to pinpoint the genetic mutation and identify the precise disease subtype is essential for early prognosis (including prenatal), disease management, and genetic counselling.
Typically, diagnosis involves collecting a biopsy for microscopic and DNA analyses of a particular gene, but these are laborious and expensive techniques, and incapable of finding the culprit mutation in 15% of cases.
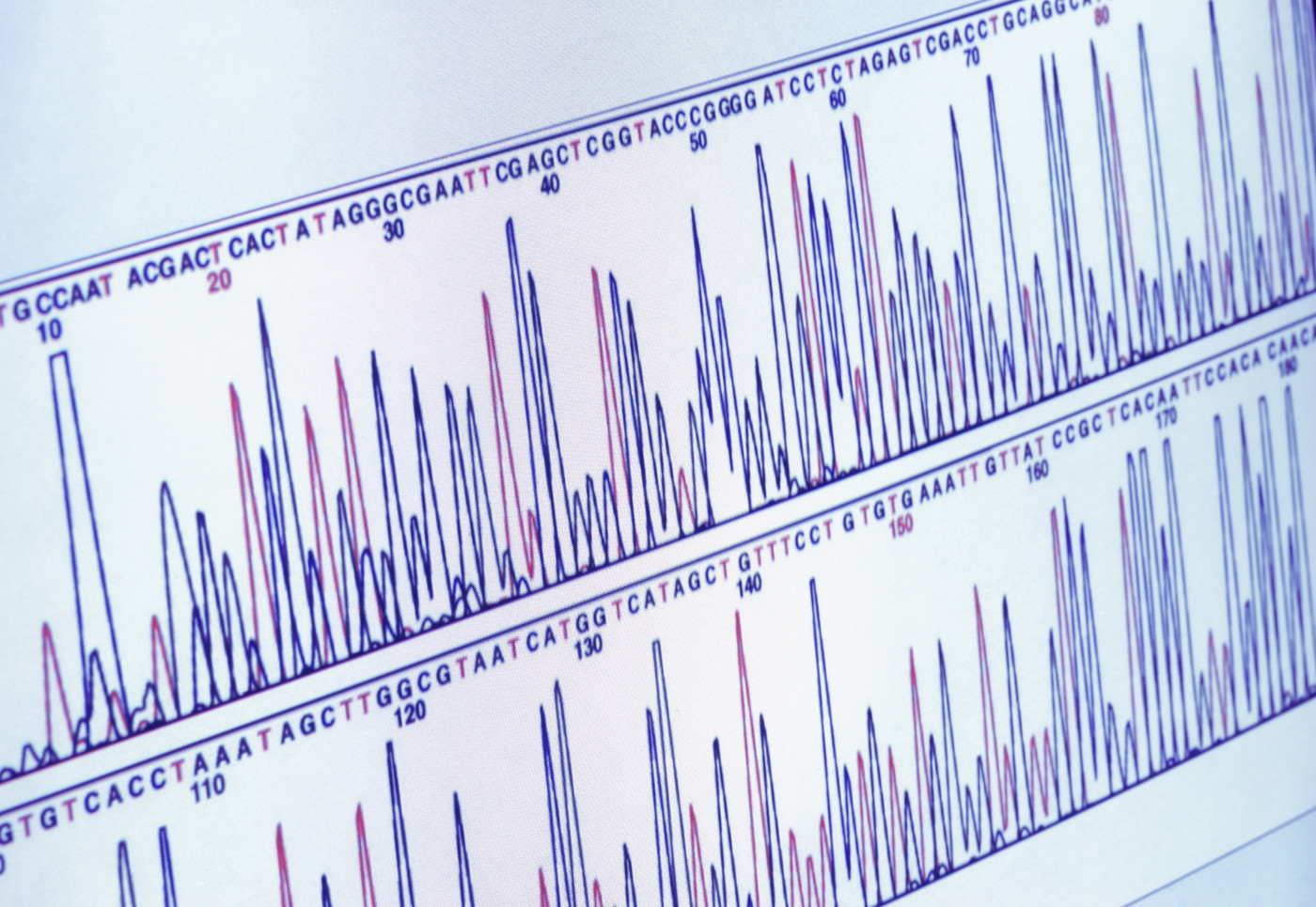
A technique used to decipher the DNA sequence, called next-generation sequencing (NGS), is able to determine the sequence of DNA quickly and efficiently. The technique is being increasingly used to diagnose genetic diseases with overlapping symptoms, such as EB.
In this case report, researchers describe a Chinese male infant with suspected EB. Within 10 days after birth, the baby had a large blister on the left lower limb, and erosions around fingertips and toe tips at birth. With time, the disease worsened and lesions spread all over his body, including the scalp, ear, hands, and feet. Fingers and toes developed pus, and eventually two fingernails were lost.
Clinicians suspected EB so they conducted NGS analysis to identify the disease subtype. The baby ended up dying close to eight weeks of age due to disease-related complications.
Targeted NGS was performed on a blood sample for nine known candidate genes associated with EB: the KRT5, KRT14, PLEC, ITGB4, LAMB3, COL17A1, LAMC2, LAMA3, and ITGA6 genes.
Mutations of the LAMB3 gene are among the known causes of junctional EB — the most severe type of EB. The gene has instructions to make one of the subunits of the laminin-332 protein, a key protein to maintain the structure of the skin with all its layers. Mutations lead to a faulty laminin-332 protein, causing extensive blistering of the skin and mucus membranes, and ultimately premature death.
Two mutations in the LAMB3 gene were identified in the baby’s DNA, including one that had never been described. Researchers then analyzed the DNA of the baby’s parents, and found that the novel gene mutation was carried by the father, whereas the mother had the previously known mutation.
In a second pregnancy, the couple wanted to know the risk of their child carrying the LAMB3 gene mutations. Thus, at 18 weeks of gestation, a sample of amniotic fluid (the fluid that surrounds the baby in the womb) was collected to isolate DNA of the developing baby. The analysis showed that the fetus carried none of the parents’ mutations.
This case report highlights how NGS can help identify new mutations underlying EB, which can improve diagnosis even at prenatal stages.
“Targeted capture sequencing is a valuable method to illustrate precise molecular pathology in patients with EB disorders, especially at an early stage of the clinical evaluation of complex disorders to avoid unnecessary and economically wasteful tests,” the study concluded.






