Adenine Base Editor Fixed Mutation in Cells From RDEB Patient
The repair to the COL7A1 gene restored type VII collagen production
Written by |
An adenine base editor (ABE), a kind of molecular tool, was used to fix a disease-causing mutation in lab-grown fibroblasts from a person with dystrophic epidermolysis bullosa (DEB).
The fix restored production of type VII collagen (C7), the protein missing in the disease, a study found.
If the findings could be translated to the clinic, they could provide a way to “reverse the root genetic cause [of the disease], potentially providing one-time cures,” the researchers wrote.
The study, “ABE8e adenine base editor precisely and efficiently corrects a recurrent COL7A1 nonsense mutation,” was published in Scientific Reports.
Epidermolysis bullosa occurs when the skin and the mucosa (a membrane that lines or covers the internal organs in the body) become too fragile, causing them to blister easily.
DEB is caused by mutations in COL7A1, a gene that provides instructions for making part of C7. There’s currently no cure for DEB, but scientists are working with gene therapy to replace the disease-causing gene.
Researchers from King’s College London, U.K. and other institutions developed a molecular tool that could edit the COL7A1 gene and turn on the production of C7 .
In a previous study, the ABE approach was able to edit a disease-causing mutation in about one-quarter of cells with two faulty gene copies. There were no off-target edits, which means the approach was precise.
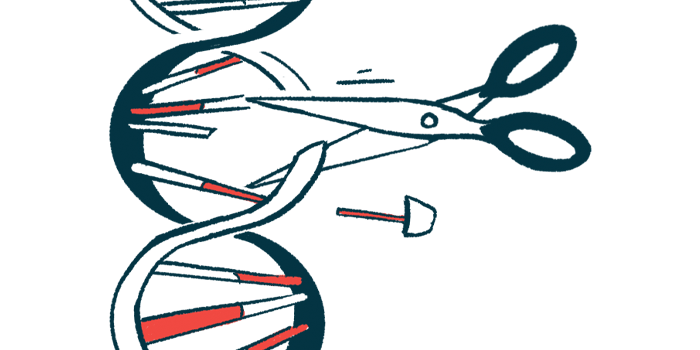
Unlike other gene editors, an ABE can make edits to a single building block (adenine) in DNA without causing so-called double-stranded DNA breaks. This means it’s able to avoid cutting through both “side rails” of the DNA’s twisted “ladder,” which may result in unexpected genetic changes and unwanted chromosome abnormalities.
The team now used ABE8e, an improved version of ABE that’s expected to be more efficient while keeping off-target effects at their lowest.
They tested ABE8e in fibroblasts from a patient with recessive DEB who carried one copy of the c.5047C>T mutation and one copy of another mutation called c.7344+1G>A, both in the COL7A1 gene. Fibroblasts are cells in the skin that make connective tissue and are critical for wound healing. They’re major producers of C7.
ABE8e’s target was c.5047C>T, a mutation reported in patients worldwide, “demonstrating the global relevance of targeting this mutation and the opportunity to recruit participants for future clinical study,” the team wrote. It leads to a shorter messenger RNA molecule — the DNA-derived template that guides protein production — and no C7 production.
When they introduced ABE8e into the fibroblasts, the c.5047C>T mutation was fixed in most (94.6%). After surveying other spots in the DNA where ABE8e could have made edits, no unintended changes were found, which means there were no off-target effects.
The researchers then found that using ABE8e in recessive DEB fibroblasts helped to significantly increase C7 production in a model called 3D human skin equivalents to levels close to normal.
“We have established a highly efficient pipeline for gene correction in primary fibroblasts with a favorable safety profile,” they said, adding their work “lays a foundation for developing therapies for RDEB patients.”