Cell and gene therapy approach shows promise for EB children
Combining treatments seen to help patients with airway involvement: Study
Written by |
In children with epidermolysis bullosa (EB) with airway involvement, a new strategy using both cell and gene therapy showed promise in a new study.
Specifically, the reintroduction of the LAMA3 gene that codes for part of a protein called laminin 332 restored the ability of cells to form a healthy barrier in airway stem cells, according to researchers. Laminin 332 is key for maintaining the skin’s integrity.
“Overall, our study provides early proof-of-principle data for a [viral]-based combined cell and gene therapy for patients with airway manifestations of EB,” the researchers wrote.
Their study, “Lentiviral expression of wildtype LAMA3 restores cell adhesion in airway basal cells from children with epidermolysis bullosa,” was published in the journal Molecular Therapy.
EB is characterized by fragile, easily blistering skin, but in certain cases, blistering also can affect internal organs.
Study shows early proof-of-principle data for combined gene and cell therapy
In cases of EB, a group of rare skin disorders, involvement of the airways can be severe. It is more common among patients with junctional EB, known as JEB, a moderate to severe form of EB.
Airway involvement is mainly found in two JEB subtypes, JEB severe and laryngo-onycho-cutaneous syndrome (LOC syndrome), which are caused by mutations in genes implicated in holding the skin layers together. Both JEB severe and LOC syndrome can be caused by mutations in the LAMA3 gene.
To date, a limited number of studies have reported airway involvement in EB.
To address this knowledge gap, a team of researchers from the Great Ormond Street Hospital for Children, in London, described a group of EB patients with airway involvement who were followed at their center between 1992 and 2023.
In total, 15 of 16 patients had airway involvement. JEB severe was the most common subtype, seen is nine patients, followed by LOC in four. Complete follow-up — from referral to being alive at study conclusion, having died, or having transitioned to adult services — was available for 15 patients, ranging from 10 months to 16.5 years.
Several patients underwent microlaryngoscopy procedures, in which a long tube with a camera is used to examine the airway, and tracheostomy to help them breathe. At the time this study was written, eight patients had died, five of whom had undergone tracheostomy.
“Although airway manifestations within EB are rare, the affected subgroup suffers from high morbidity and an inexorable worsening of both quality of life and life expectancy,” the researchers wrote.
Genetic analyses were available for 15 patients; 10 were positive for at least one disease-causing mutation in the LAMA3 gene. Seven patients had mutations affecting both LAMA3 copies and two had mutations in one copy. Another patient had the same mutation in both copies of the LAMB3 gene and another mutation in a copy of LAMA3.
The remaining five patients had disease-causing mutations in LAMB3, another laminin-coding gene, or other genes important for skin structure.
Tissue from the airways of 5 children used to generate cell culture
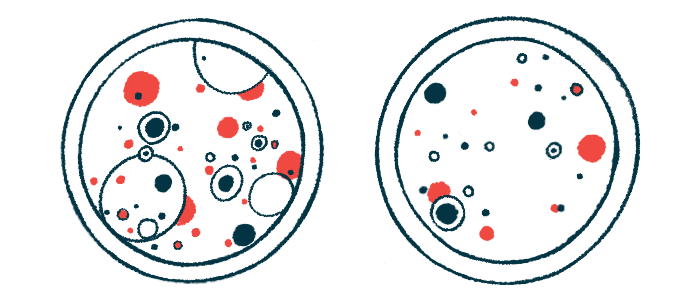
The researchers then used tissue from the airway of five children to generate a cell culture. They successfully established these cultures from windpipe (trachea) and larynx (voice box) samples from four patients. The other participant was a child without EB, who served as a control.
The results showed that the levels of the LAMA3 protein were severely reduced in EB cells compared with that from the control. EB-derived cultures also showed cell adhesion defects.
Using a viral vector as a vehicle, the scientists then introduced a healthy version of the LAMA3 gene. Further analysis confirmed that the gene had been successfully integrated in the target cells, and was now producing significantly higher messenger RNA and protein levels of LAMA3. Messenger RNA is generated from DNA and serves as a template for protein production.
The ability of the LAMA3-expressing cells to form a functional barrier was within the normal range of what was seen for non-EB cells, as shown by the values of transepithelial electrical resistance (TEER). TEER is a well-established method for measuring electrical resistance across a layer of cells, which informs on barrier integrity. The cells also were able to mature and reach comparable adhesion levels relative to the non-EB cells, the data showed.